Research Article
Brainstem Cavernoma: Wath Management?
1366
Views & Citations366
Likes & Shares
Management of brain stem cavernoma is not common in neurosurgery. Controversial opinions are reported in literature. The authors report the case of a 34 years old patient treated for a brain stem cavernoma. Therapeutic issues relative to this entity are reviewed and discussed through this paper.
Material and methods: A 34 years old male patient with no medical background who was complaining about limbs paresthesia followed by left leg weakness leading to gait disturbance had been hospitalized.
Outcomes: Imaging studies showed a right-sided pontine cavernous malformation with hemorrhage. A stereotactic biopsy and a surgical excision were performed with good result.
Conclusion: Surgical excision of symptomatic brain stem cavernoma is a challenging surgery and represent the most advantageous alternative. An experienced team may achieve this without worsening the patient.
Keywords: Brain stem cavernoma, Hemorrhage, Stereotactic biopsy, Robot
INTRODUCTION
Brain stem cavernoma is a special entity most often revealed by hemorrhage. Its management is subject to controversies. Surgical excision of brain stem cavernoma is one of the most challenging surgery. The authors report a pontine cavernoma in a 34 years old patient without medical background. Therapeutic issues relative to this entity are reviewed and discussed through this paper.
CASE REPORT
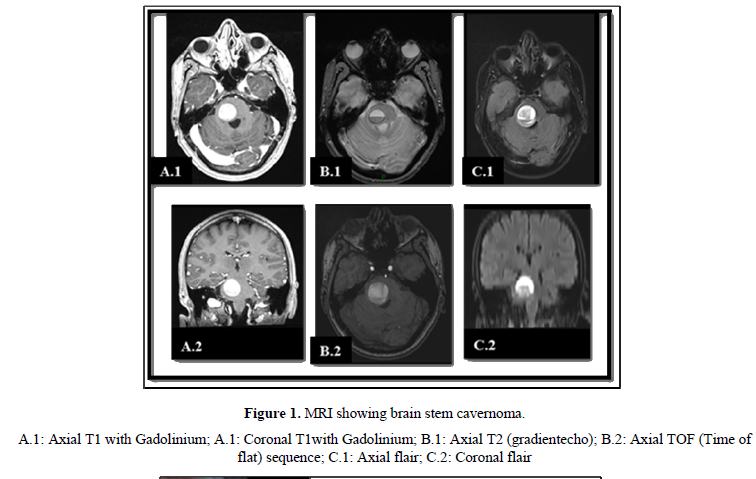
A 34 years old male patient with no medical background was complaining about limbs paresthesia followed in a week by left leg hypoesthesia and weakness leading to gait disturbance. The cerebral CT scan shows an acute pontine bleeding on the right side. The patient had been hospitalized for betamethasone corticosteroid therapy that decreased motors issues. After that he was released for a home follow up. Two months later he came for moderate headaches, swallowing issues, dizziness, diplopia and left sided weakness. The cerebral MRI demonstrated a pontine well definite lesion of about 29 x 26 mm (Figure 1), hyper intense on T1 weighted, hypo signal surrounding rim on T2 weighted and a blooming pattern on SW1. It also showed on diffusion sequences some surrounding artifact of blood degradation products. There was a slight mass effect on the fourth ventricle without any upstream hydrocephalus. These imaging characteristics strongly suggested a pontine cavernous malformation.
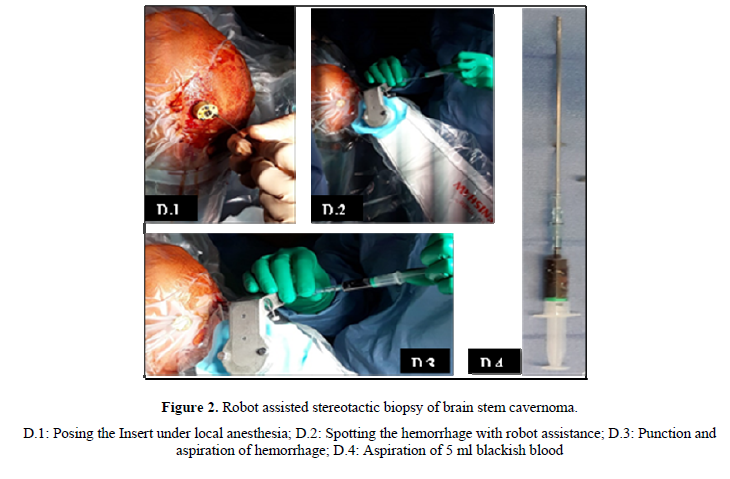
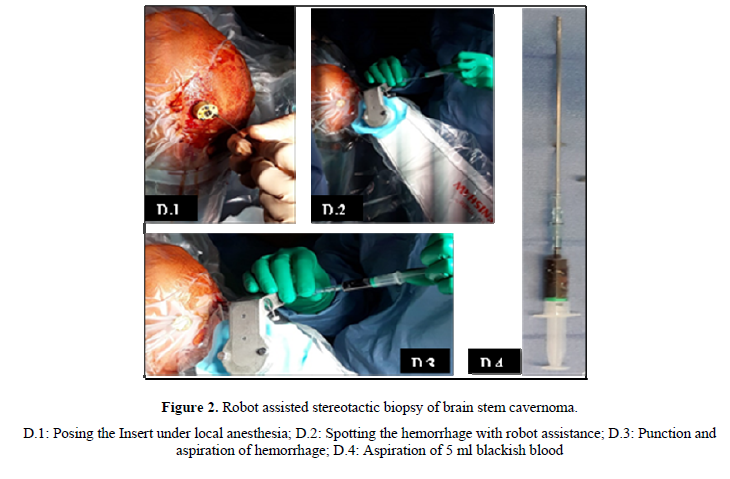
A robot assisted stereotactic biopsy was performed (Figure 2) and brought back 5 ml of blackish blood. Post-operative period was uneventful and the patient showed slight improvement of dizziness, motor and swallowing issues. Postoperative CT scan showed an important hemorrhage residue.
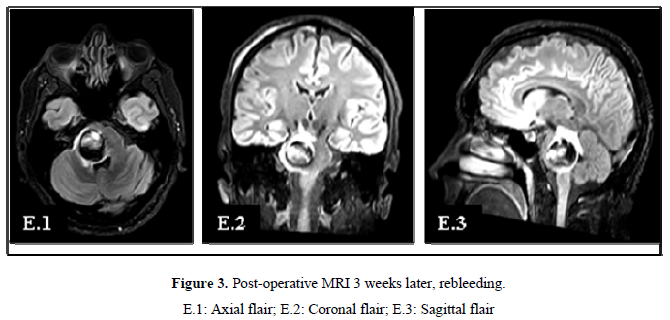
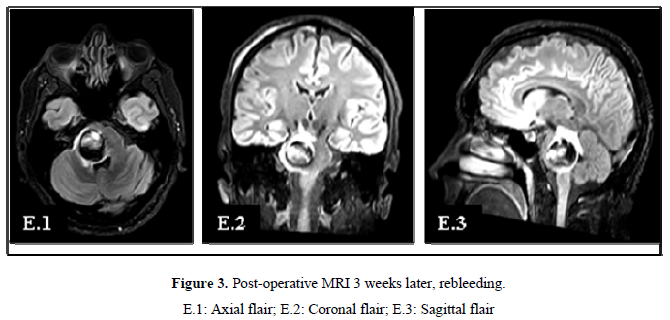
Three weeks later the patient came with worsening of left-sided motor weakness, swallowing issues, nausea and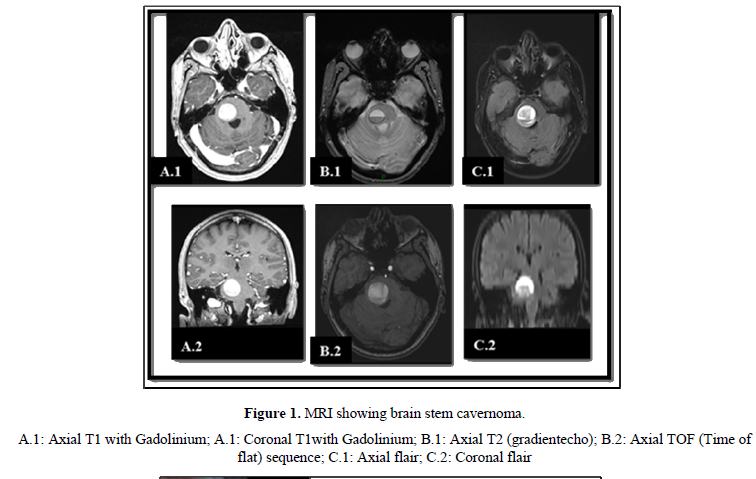
DISCUSSION
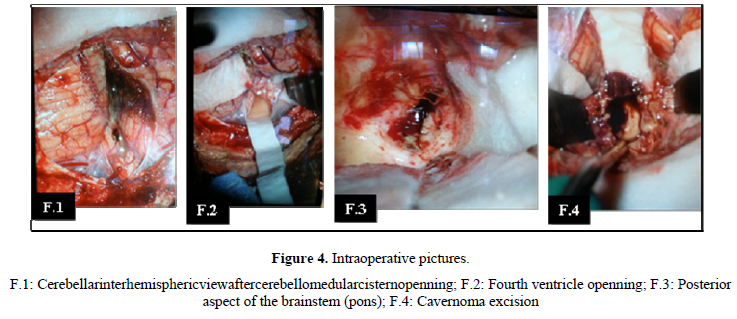
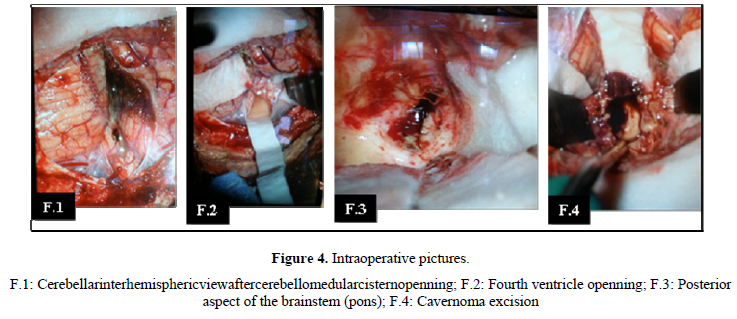
Cerebral cavernous malformations developing 0, 4 -0, 9% of population and comprise 8-15% of central nervous system vascularmal formations [1]. Brain stem cavernoma occurs in about 9-35% [2,3] Pontine location is most frequently found [2,3]. Brain stem cavernoma constitute a special entity [4] due to high rate of hemorrhage. This rate is 30 times higher than in any other locations [4]. So that sudden or progressive onset hemorrhage is the main event of diagnosis as found in our case. Dexamethasone was help full to reduce the brain stem malignant swelling. Several authors recommend administration of steroids 1-2 weeks before surgery [5]. Robot assisted stereotactic biopsy was performed because of recurrence of neurological symptoms. It was helpful to have a transitory improvement of symptoms and relieve the patient before surgery. According to Nataf [6], biopsy of cavernous malformations suggested on MRI must be avoid. Eloquent locations of brain stem cavernous mal formation makes its removal one of the most difficult surgery [4]. It is a challenge to achieve a complete surgical resection keeping other neurological structures safe. Surgical excision is indicated for accessible cavernoma with prior hemorrhage [6]. However, there is no codified surgical procedure for brain stem cavernoma. There are several opinions about indications and timing of surgery [7]. Some authors recommend micro surgical removal for cavernoma with prior bleeding and worsening of neurological impairment [8]. Others are for surgery in every patient even asymptomatic one [9]. In our opinion, surgical treatment for asymptomatic patients is excessive. Niranjana et al. recommend surgery in acute period or 4-6 weeks later [10]. According to them, in early phase of bleeding a cleavage plane between hemorrhage and surrounding healthy tissue exists. Several approaches are proposed (5; 7). The appropriate one depends on the relationship between cavernoma and brain stem’spial and ependymal surface [7]. Infratentorial supracerebellar approach is one of the most privileged surgical procedure [7]. We choose an infratentorial cerebellar interhemispheric approach in semi-sitting position in our case. It was helpful for a good excision with no worsening of patient symptoms. Mortality rate correlates to neurosurgeon’s experience (1; 11). The rebleeding occurs in 43 - 44% and can be prevented by a complete surgical resection (7; 12). This rate is higher a month after surgery [2]. Incomplete resection may occur with a non-experienced surgeon. The higher the series the lower is the rate of incomplete resection [2,5].
CONCLUSION
Surgical excision is the best treatment of brain stem cavernoma. It is a challenge addressed by experienced neurosurgeons. Good surgery with a few sequelae is possible. Management of this affection needs to be codified.
- Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, et al. (2002) Cerebral cavernomas in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25(1-53): 1-25.
- Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, et al. (1999) Cavernous malformations of the brainstem: Expérience with 100 patients. J Neurosurg 90(1): 50-58.
- Hsu FP, Rigamonti D, Huhn SL (1993) Award IA, Barrow DL, editors. Cavernous malformations. Park Ridge: AANS: 13-23.
- Isolan G, Antunes A, Aires R, Geogeto SM, Tahara A, et al. (2012) Brain stem cavernomas: À surgical challenge. Einstein (Sao Paulo) 10(1): 67-73.
- Wang CC, Liu A, Zhang JT, Sun B, Zhao YL (2003) Surgical management of brain stem cavernomas malformations: Report of 137 cases. Surg Neurol 59: 444-454.
- Nataf F, Roux FX, Devaux B, Page P, Turak B, et al. (2007) Brainstem cavernomas: Surgical experience at the CH Sainte-Anne general hospital. Neurochirurgie 53(2-3): 192-201.
- Bozinov O, Hatano T, Sarnthein J, Burkhardt JK, Bertalanff H (2010) Current clinical management of brainstem cavernomas. Swiss Med Wkly 140: W13120.
- Steinberg GK, Chang SD, Gewirtz RJ, Lopez JR (2000) Microsurgical resection of brainstem, thalamic, and basal ganglia angiographically occult vascular malformations. Neurosurgery 46(2): 260-270.
- Sindou M, Yada J, Salord F (2000) Functional results after microsurgical resection of brain stem cavernous malformations (retrospective study of a 12-patient series and review of the recent literature). Acta Neurochir (Wien) 142(8): 843-852.
- Niranjana R, Tsukasa K, Ameen AM, Liew BS (2019) Timing of surgery and surgical strategies in symptomatic brainstem cavernomas: Review of the literature. Asian J Neurosurg 14(1): 15.
- Bertalanffy H, Gilsbach JM, Eggert HR, Seeger W (1991) Microsurgery of deep-seated cavernous angiomas: Report of 26 cases. Acta Neurochir (Wien) 108: 91-99.
- Cenzato M, Stefini R, Ambrosic C, Giovanelli M (2008) Post-operative remnants of brainstem cavernomas: Incidence, risk factors and management. Acta Neurochir (Wien) 150(9): 879-886.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- BioMed Research Journal (ISSN:2578-8892)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Journal of Rheumatology Research (ISSN:2641-6999)
- Chemotherapy Research Journal (ISSN:2642-0236)
- International Journal of Diabetes (ISSN: 2644-3031)
- Advance Research on Alzheimers and Parkinsons Disease





